Pre-Surgical Risk Stratification using Deep Learning on 12-lead ECGs for Non-Cardiac Populations
- Program: Biomedical Engineering
- Course: EN.580.480 Precision Care Medicine
Project Description:
Surgical decision-making is critically dependent on accurate assessments of risk, but the effectiveness of electrocardiography (ECG) in evaluating surgical risks remains unclear, despite its common use in clinical settings.
Using 12-lead diagnostic ECG taken prior to major noncardiac surgery in 28,661 adult patients enrolled in the MIMIC-IV dataset, we trained a series of convolutional neural network (CNN)-based models to predict major post-surgical adverse outcomes including acute myocardial infarction (MI), in-hospital mortality (IHM), and a composite of MI, 30-day mortality, and stroke (composite). These waveform-only models achieved comparable discrimination to the Revised Cardiac Risk Index (RCRI), a benchmark pre-surgical risk stratification tool used to evaluate non-cardiac surgical candidates. We then integrated ECG waveforms with a small number of clinical variables (age, sex, and RCRI components) to create a fusion model. To gain insight on the explainability of the models, we generate counterfactual ECGs using generative adversarial networks.
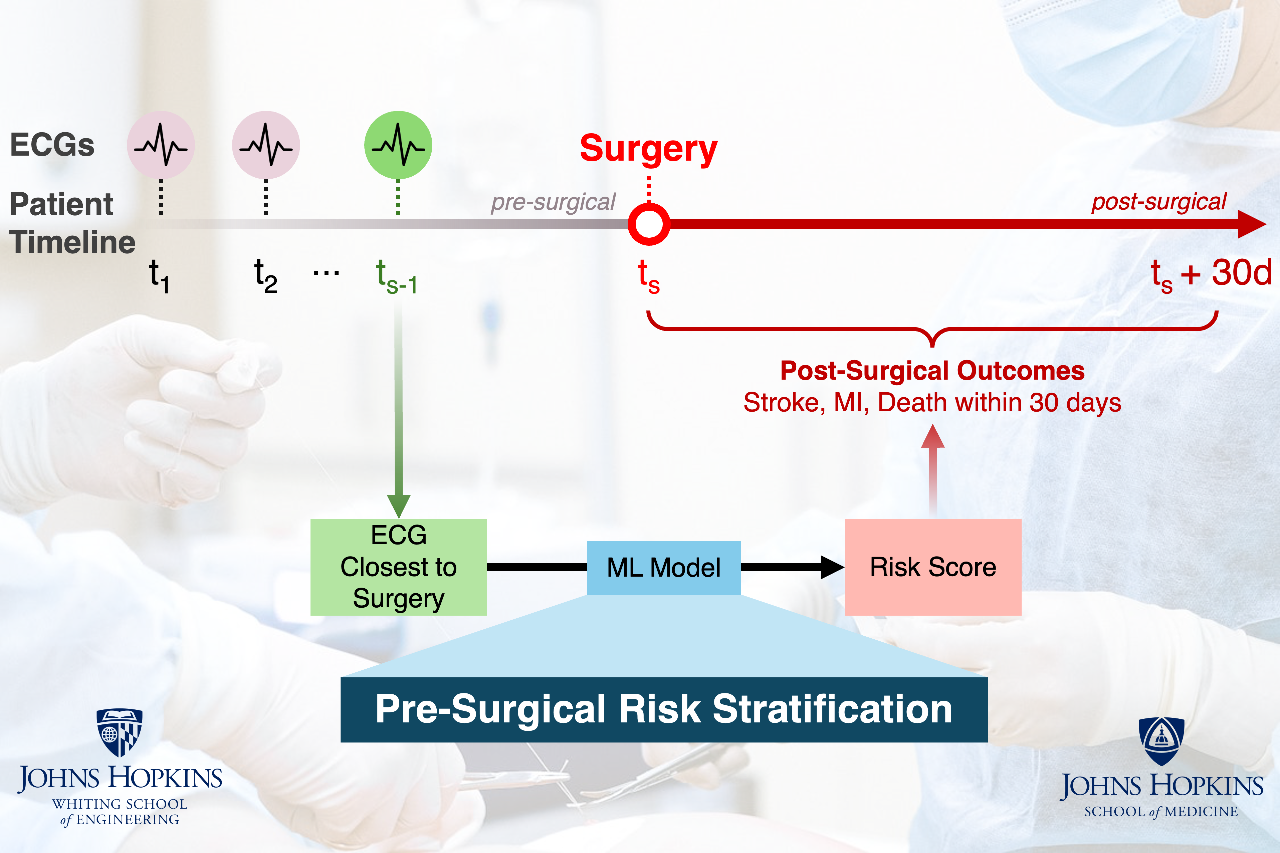
Project Photo:
We aim to create a deep learning model that improves methods for analyzing ECG signals to predict surgical risks like myocardial infarction, stroke, and death. To explain how the model evaluates ECGs, combines this with tabular data, and calculates a risk score, we will use a counterfactual explanation approach.
Project Poster
 Open full size poster in new tab (PDF)
Open full size poster in new tab (PDF)
Project Post Summary:
Surgical decision-making is critically dependent on an accurate assessment of risk. Despite routine use of electrocardiography (ECG) in the clinical setting, the value of this test in surgical risk stratification is not well understood. Using 12-lead diagnostic ECG taken prior to major noncardiac surgery in 28,661 adult patients enrolled in the MIMIC-IV dataset, we trained a series of convolutional neural network (CNN)-based models to predict major post-surgical adverse outcomes including acute myocardial infarction (MI), in-hospital mortality (IHM), and a composite of MI, 30-day mortality, and stroke (composite). These waveform-only models achieved comparable discrimination to the Revised Cardiac Risk Index (RCRI), a benchmark pre-surgical risk stratification tool used to evaluate non-cardiac surgical candidates. We then integrated ECG waveforms with a small number of clinical variables (age, sex, and RCRI components, routinely collected clinical variables) to create a fusion model. The fusion model achieved an AUROC of 0.866 (95% CI [0.851, 0.880]), 0.898 (95% CI [0.887, 0.908]), and 0.832 (95% CI [0.824, 0.841]) for MI, IHM, and composite, significantly outperforming models based on ECG waveforms (MI: p=0.001, IHM: p<10^(-4), composite: p<10^(-4)) or RCRI alone (MI: p<10^(-4) for all outcomes). To gain insight on the explainability of the models, we generate counterfactual ECGs using generative adversarial networks. Given an input ECG, our explainability module produces a set of plausible modifications to the waveform that allows us to visualize morphological differences relevant to the outcome classification verdict. We then show that these counterfactual ECGs provide credible explanations for classifier decisions.
Course Faculty
- Joseph L Greenstein
- Casey Overby Taylor