Early Dynamic Prediction of Organ System Deterioration in ICU Patients
- Program: Biomedical Engineering
- Course: EN.580.480 Precision Care Medicine
Project Description:
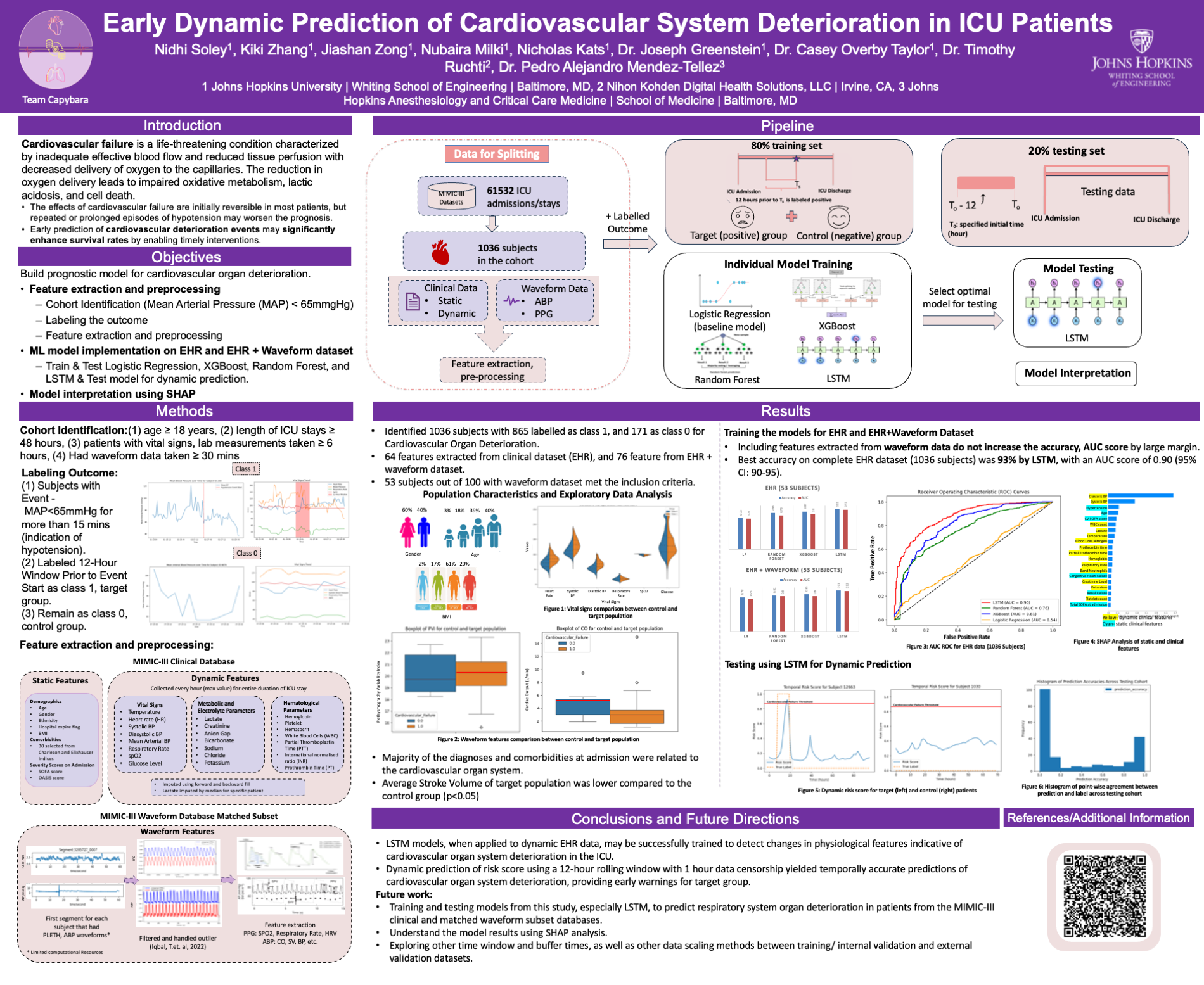
Cardiovascular and respiratory deterioration signify progressive decline in respective organ systems, with cardiovascular (CVS) issues accounting for 17.8% of ICU deaths and pulmonary failure 1.1% (Mayr et al., 2006; Norness et al., 2021). Current models often focus on singular organ outcomes or static inputs, failing to capture dynamic ICU patient data (Hu J. et al., 2022). In this project we built prognostic model for cardiovascular (MAP<65mmHg) and acute hypoxemic respiratory (need of mechanical ventilation) organ deterioration separately. Our project developed prognostic models for cardiovascular and acute hypoxemic respiratory deterioration separately, leveraging MIMIC III data. We identified 1036 patients meeting criteria and extracted relevant features. We divide the complete dataset into training and test sets by randomly splitting in an 80:20 ratio in a stratified manner. Training diverse machine learning models, including Logistic Regression, Random Forest, XGBoost, and LSTM, we achieved promising accuracy (93%) and AUC (0.90, 95%CI: 90-95) with LSTM on EHR data. The model gave higher risk score and crossed the threshold before the event start for patients in target to give an early warning. Dynamic risk prediction using a 12-hour rolling window showed temporal accuracy, providing early warnings. Future endeavors will explore varying time windows, buffer times, and data scaling methods, extending the model to predict respiratory deterioration.
Project Poster
 Open full size poster in new tab (PDF)
Open full size poster in new tab (PDF)
Project Post Summary:
Our project used the MIMIC-III Waveform Database Matched Subset to develop a model that predicts cardiovascular system deterioration in the ICU. Our metric for this deterioration was mean arterial pressure below 65 mmHg for 15 minutes, as that is an indicator of hypertension. We extracted static and dynamic clinical data along with waveform information from arterial blood gas and photoplethysmogram waves. We divided our cohort of 1036 patients into 80% for training and 20% for testing. Four machine learning models were trained on both electronic health record (EHR) data and EHR combined with waveform data. The most accurate model, LSTM, was turned into a dynamic prediction risk score. Dynamic risk prediction using a 12-hour rolling window showed temporal accuracy, providing early warnings. This score can help detect changes in patients’ physiological features, signaling potential cardiovascular system deterioration in the ICU.
Course Faculty
- Joseph L Greenstein
- Casey Overby Taylor
Project Mentors, Sponsors, and Partners
- Pedro Alejandro Mendez-Tellez
- Timothy Ruchti